Recent Articles
Safety Tips for this Gardening Season Apr 16, 2024
The Role of Stretching and Flexibility Exercises Apr 8, 2024
Hydration and Orthopaedic Wellness: Why Water Matters Mar 25, 2024
Fueling your Body: Using Nutrition to Benefit Musculoskeletal Health Mar 12, 2024
How Orthopaedic Associates's Team Practices Living in Motion Feb 29, 2024
A Better Move for Motion Feb 22, 2024
Orthopedic Issues and Diabetes: Understanding the Connection Dec 13, 2023
Our Recipe for Joint Health Nov 28, 2023
Orthopaedic Associates Begins Partnership with New Rock Ridge High School Oct 2, 2023
Getting You Back in the Game after an ACL Injury Sep 12, 2023
How Cold Weather Affects Joint Pain
December 14, 2021
Do you seem to know when colder weather is coming because you can “feel it in your bones”? Many patients experience flare-ups of joint pain at the start of the winter season. While there is no one explanation for this link between the change of temperature and joint pain, we do know of a few possible reasons why you may be feeling these effects.
Barometric Pressure and Weather
Barometric pressure is the measurement of air pressure in the atmosphere. This measurement changes constantly and is dependent on where the reading is taking place. Weather also changes with barometric pressure, meaning that the pressure reading will often fall before cold weather sets in. Aspects of the weather, including precipitation, humidity, and temperature are all at play here, making it difficult for scientists to be sure what exactly causes the additional pain.
One theory is that when the cartilage that cushions the bones inside the joint is worn away, like for those with arthritis, nerves within the exposed bones feel the changes in barometric pressure.
Another theory is that changes in barometric pressure can make tendons, muscles, and scar tissue expand and contract - creating pain in the joints.
Dropping temperatures can also make the fluid inside of your joints thicker, making them feel stiffer. Joints may also stiffen up due to a lack of movement, which often happens when people stay indoors and are inactive due to colder weather.
How to Ease Joint Pain
There are multiple methods that you can use to ease weather related joint pain.
As the weather becomes colder, keep yourself warm by using electric blankets, wearing warm clothing and layering, keeping your house well heated, and making sure you are warming up your car before use.
You can also help prevent your joints from swelling by wearing well-fitted gloves that keep fluid out and by wearing knee braces. To help relax muscles, apply heating pads to painful areas when necessary.
Trying to stay active will also help to reduce joint pain. Keep joints limber and strong by practicing a few stretches and gentle exercises like swimming or yoga every day.
A doctor may also recommend taking pain medication. Consult with your doctor before taking any medications to ensure correct type and dosage.
When to See a Doctor
Consult your physician if you experience unusual or new symptoms. These may include swelling, redness, or difficulty putting pressure on or using a joint.
If you are unable to ease joint pain, contact our physical therapy team or your physician for alternative suggestions or treatments.
National Physical Therapy Month
October 21, 2021
October is National Physical Therapy Month, and in celebration we would like to take this opportunity to raise awareness in regards to the benefits of physical therapy and the pride Orthopaedic Associates’ therapists have in the work they do and help they provide.
Physical therapy helps patients get back to their active lifestyle after an injury or illness by assessing and diagnosing their physical deficits in combination with mechanical restrictions then putting together a personalized treatment approach in conjunction with working directly with a physician. Physical therapists aim to ease pain and help you move, function, and live better by working by your side through all stages of healing - from diagnosis through recovery.
Patients may seek physical therapy for numerous reasons including; to relieve pain, to improve movement or ability, to rehab after a stroke, accident, or surgery, to prevent or recover from a sports injury, to manage a chronic illness, as well as many other health problems. People of all ages are proven to benefit from physical therapy.
If a patient has a serious injury or illness, a physical therapist does not take the place of a doctor or surgeon, however they can work closely with other healthcare professionals to create and guide treatments to better outcomes.
The therapists at Orthopaedic Associates enjoy getting to know each patient. Building that relationship and rapport is important so that they can learn what progress the patient wants to make and what kind of activities they want to get back to.
During the first session, your physical therapist will examine and assess your needs by asking questions regarding pain or other symptoms, ability to move and do everyday tasks, as well as other medical history that is relevant. They will also administer a series of tests. Doing this helps to diagnose a condition, understand why you have the condition, and develop a treatment plan that works for you.
At OAD, patients typically meet with their therapist and their surgeon at the first appointment. From there we can talk about the plan of care and what the expectation of the patient and OAD’s team is.
Treatments could include guided stretches or exercises, massage, cold or heat therapy, practice with canes, walkers, or other items to help with movement and balance, or rehab to help learn the use of an artificial limb. A therapist will assess progress and adjust treatment when necessary.
One advantage a patient will experience at Orthopaedic Associates is our offering of a one-on-one treatment approach. Patients will be generally seen from start to finish of treatment by one physical or occupational therapist - so that they aren't bounced around from one to the next.
Another advantage is the direct access OAD therapists have with their physicians. This connection bridges the gaps where things could potentially slip through. It is important for patients to know that this connected loop does not get dropped and care team members are continually in communication. From day one the therapists are well aware of what occurred in surgery and can have that communication with the surgeon being literally steps away from each other. This communication goes both ways where if there is a question on the physician's end they can come speak with one of the physical therapists and vice versa.
Orthopaedic Associates of Duluth has several specialized programs including a sports metrics program which works with athletes both in preventing injuries specifically with the ACL and preventing reinjury with the ACL. Another program is our return to sport testing which can be for any injury whether it is a lower or upper body injury to make sure the athlete is safe to return to their sport. We also offer a running assessment, which is also meant to prevent running injuries or can treat runners who have had an injury in the past and get them back to their love of running.
Learn more about our team of therapists, each having extensive education in the areas of orthopedics, manual therapy, sports rehab, and injury prevention by visiting www.oaduluth.com/therapy.php. Please request an appointment if you feel your life and health would benefit from physical therapy.
The Risk of Delaying a Total Knee Replacement
September 23, 2021
We understand the appeal you might see in putting off a surgery. Maybe your life is busy and you are waiting for a quieter time, maybe you have fears about the procedure or are concerned about the recovery process, or maybe you just haven’t made the time to call to schedule your appointment. Studies show that up to 90% of individuals who need a knee replacement wait too long, however delaying the procedure could deprive patients of a surgery’s full potential or cause greater pain.
When a patient waits too long for a knee replacement, the osteoarthritis creates continued deformity of the knee joint. This causes the body to compensate and places additional stress and strain on other parts of the body. This compensation can affect your muscles and ligaments, skeletal system, hips, and even your good knee.
Deterioration of function can also lead to the inability to be active, which can lead to additional problems due to weight gain, low endurance, cardiac conditions, or emotional health. This can also slow down the recovery process and can make post-operative procedures, like physical therapy, more challenging.
As the joint deteriorates while delaying a total knee replacement, the overall replacement process can become more complicated. The surgeon will need to navigate the increased deformity of the joint while operating. This leads to a longer surgery, resulting in a higher risk of postoperative concerns including blood clots or infections.
Patients who wait longer also do not tend to get as much function back after surgery as someone who had it sooner. A good indicator of expected motion after surgery is the mobility of the knee before replacement.
While one reason patients put off a surgery is to postpone an unpleasant experience, by delaying you are ultimately dealing with chronic pain for a longer period of time, which affects your quality of life. As months or even years go on, you are also aging. With age comes longer and more difficult recovery times as well as other health issues that may affect a surgery. The younger and healthier a patient is at the time of surgery is typically a good indication of how well surgery and recovery will go.
When hesitant to schedule a joint replacement surgery, remember that knee replacement is one of the most successful surgical procedures. At Orthopaedic Associates, we use cutting-edge, minimally invasive techniques in a comfortable setting with the best team in the region to ensure the best possible experience, recovery, and outcome. Learn more about our joint replacement services at www.oaduluth.com/joint-replacement-specialists.php.
It is important to stay proactive when it comes to a total knee replacement. Make an appointment by calling (218) 722-5513 to consult your doctor or orthopaedic surgeon and talk about your best options to help you live in motion.
How to Gear up for an Injury Free Fall Sports Season
August 20, 2021
According to data from the National Safety Council, young people aged 5 to 14 account for 50% of football injuries, 45% of soccer injuries, and 40% of lacrosse and rugby injuries treated in emergency rooms in 2017. Another statistic to note is that each year about 1.35 million student-athletes suffer injuries while playing sports. With this data in mind, it is important that while students are practicing for their fall sports, they should also be practicing good habits to prevent injury, especially after the long summer break or even longer break due to the pandemic.
Many fall sports including soccer, football, and cross country have running at their core. Other sports like tennis, lacrosse, and volleyball focus more on strong, repetitive motions. Both strength and cardiovascular training are essential before and during the fall season to ensure safety and to decrease the chance of injury.
Types of Injury
One of the most common injuries seen during fall sports is concussions. In a recent study, the Brain Injury Research Institute estimated that 1.6 to 3.8 million athletes suffer from concussions annually. In sports like football where there is a high level of contact and soccer where the head is used in play, any hits to the head should be taken seriously due to the possibility of a brain injury. Playing through a concussion can lead to a more serious injury, so if an athlete is showing signs of headache, nausea or vomiting, confusion, ringing in the ears, fatigue, or head/eye pain when exposed to bright light they should seek help. If an athlete has had more than one concussion, they may also need to discuss further safety measures to avoid long-term brain distress.
Fractures, or a bone break, are also common and can include several different types, including:
Open Fractures - the bone pokes through the skin
Comminuted Fractures - a bone that has been broken more than once
Complete Fractures - the bone breaks in two
Bowing Fractures - the bone bends but doesn’t snap, typically limited to children
Greenstick Fractures - one side of the bone is cracked, while the other remains intact
These require immediate attention and often need a long break from play.
Strains happen from sudden strange movements or overuse of a muscle. Symptoms of a strain include swelling, stiffness, cramping, trouble moving, or feeling a pop. Strains should be given rest so that athletes don’t experience a worse injury from overexertion, as well as elevation and icing.
Sprains often occur in the ankle, wrist, or knee and are partial or complete tears of the ligament within a joint. They typically happen when a part of the body is twisted in an awkward way, for example, if landing incorrectly when kicking a ball. Signs of a sprain are a popping sound at the time of injury, pain in the area, swelling or bruising, difficulty walking, or a limited range of motion.
Most sprains are minor, however, an anterior cruciate ligament (ACL) tear is a common and severe injury that requires rehabilitation and surgery. An ACL tear affects the ligament that stabilizes the knee.
Strains and minor sprains are similar injuries and can be treated and healed with appropriate Protection, Rest, Ice, Compression, and Elevation - PRICE.
Tennis elbow doesn’t only occur in athletes on the tennis courts, repetitive use of the elbow in any sport can create small tears in the ligamines, leading to pain and inflammation.
Runners often can experience shin splints from overuse. Shin Splints is an injury of the soft tissues that hold the muscle to the bone and is caused by a rapid increase in intensity or frequency of running, improper shoes, training on hard services like concrete, or flat feet. While most commonly seen in cross country runners, shin splints can show up in any sport that involves a high amount of running like soccer or field hockey. Stretching before practice and making sure to rest between sessions can help prevent shin splints. Making sure to replace shoes regularly, about every 300-500 miles is also beneficial.
Rest and icing typically heal shin splints, however, in some cases, athletes need further treatment. These cases include: when a doctor suspects a stress fracture, tendonitis develops, or if shin splints are incorrectly diagnosed for a chronic exertional compartment syndrome where pressure builds up in the muscles.
It is estimated that about 40% of all sports injuries are knee injuries. Runner's knee or Patellofemoral Syndrome is an injury that causes pain when the cartilage in the kneecap becomes irritated, worn, or soft, leading to a shifting of the kneecap’s position and poor alignment. Volleyball players can experience this due to their repetitive crouching or squatting motions, however, any athlete who repeatedly moves in a way where the kneecap rubs against the leg bone can experience damage to the tissue. Other symptoms include the knee-buckling or making grinding and popping sounds. The PRICE method can also help with these symptoms, as well as kinesiology taping or bracing and physical therapy focusing on strengthening the knee, core, and surrounding muscle groups.
Preventing Injury
Simple things can help decrease the chance of a fall sport-related injury including getting a physical before the season starts to ensure health, stretching and warming up, cross-training to strengthen all muscle groups, investing in good footwear and proper protective equipment, and fueling an athlete’s body correctly. When possible, it is also beneficial to avoid concrete and to exercise on well-maintained grass or soft track surfaces.
It is also important for every athlete to remember to speak up when they are feeling pain, rest after an injury, and enjoy downtime.
Following these guidelines can prepare the body and keep young athletes off the bench this season.
If your student-athlete is experiencing pain or an injury due to a fall sport, or if you have any questions about keeping them healthy, reach out to our team to schedule an appointment!
Carpal Tunnel Syndrome Facts, Symptoms, and When to See a Doctor
July 14, 2021
The carpal tunnel is a narrow pathway surrounded by ligaments and bones on the under side of your hand. Carpal tunnel syndrome occurs when there is pressure on the median nerve, which runs through the carpal tunnel from your forearm to your hand. This nerve provides sensation to the palm side of your thumb and fingers, excluding the little finger. It also provides nerve signals to move the muscles around the base of your thumb, helping with motor function.
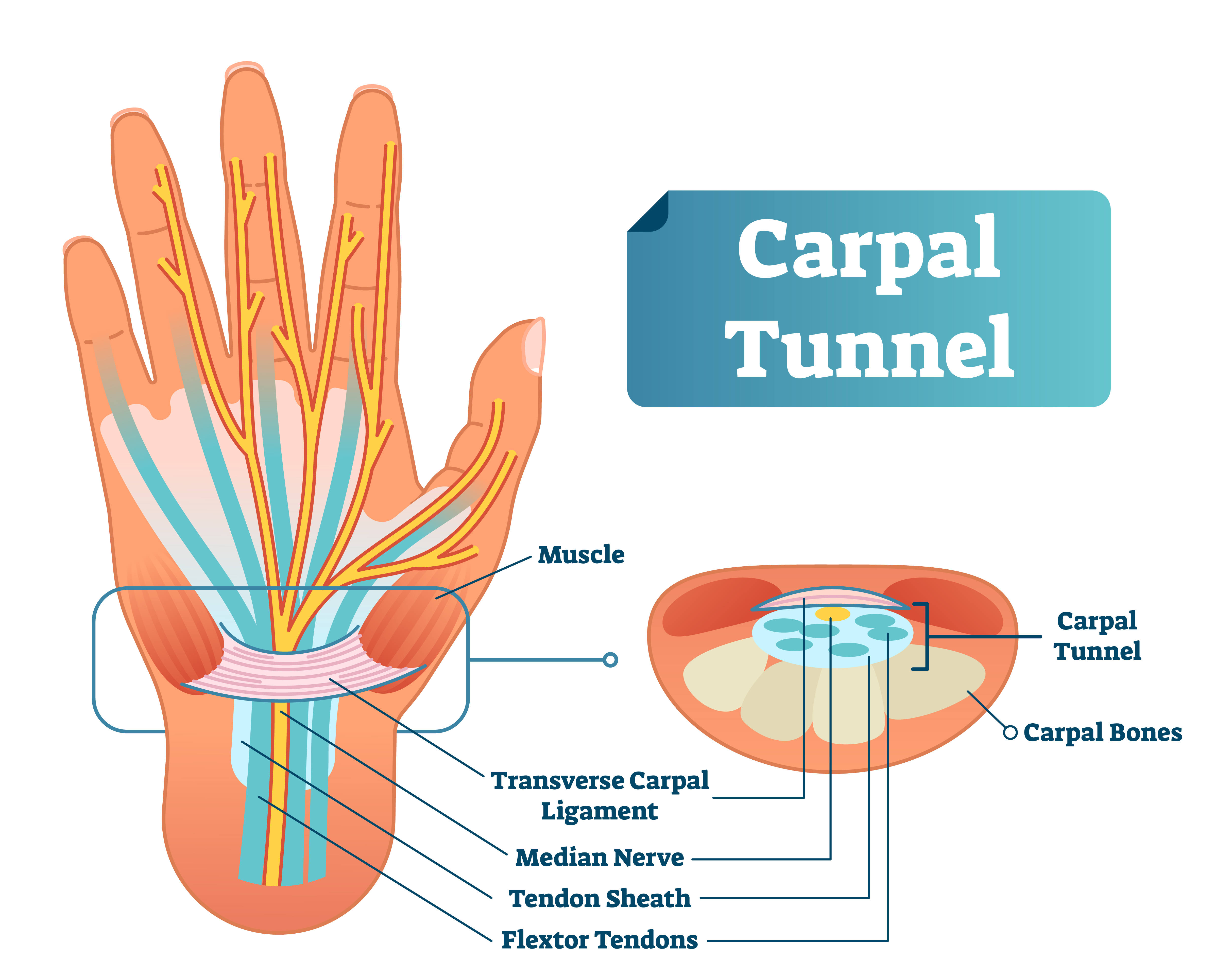
When something squeezes the median nerve in the carpal tunnel, it can cause irritation, swelling, and create issues. Often, there isn’t one single cause of carpal tunnel syndrome but instead a combination of risk factors contributing to the development of the condition. However, health problems and repetitive hand movements can contribute to experiencing carpal tunnel syndrome. Studies also show that women and older people are more likely to develop the condition.
Usually starting gradually, symptoms of carpal tunnel syndrome include numbness, tingling, shock-like sensations, or weakness affecting the thumb, index, middle, and ring fingers. These sensations may travel up your arm and are often noticed while holding something for a prolonged period of time like a steering wheel, phone, or book. Experiencing symptoms at night is often common due to people often sleeping with their wrists bent. The feeling of weakness may cause people to drop objects. This is due to the weakness of the thumb’s pinching muscles, which are also controlled by the median nerve.
To relieve caused pain, some people find that “shaking out” their hands briefly helps, however the pain or numb feelings may become more frequent and eventually constant over time. These symptoms may also wake you from sleep, interrupting good sleep patterns.
To reduce the chance of getting carpal tunnel syndrome, there are many methods you can use to minimize stress on your hands and wrists. These include, reducing force and relaxing your grip, taking short and frequent breaks when completing tasks, watching your form and improving posture, changing your computer mouse, and keeping your hands warm.
When normal activities and sleep patterns become interfered, it is time to schedule an appointment with your doctor for a diagnosis and treatment.

Your doctor will look into your history of symptoms, as well as do a physical exam if you fear you may have carpal tunnel syndrome. They may also decide x-rays, an electromyography, or a nerve conduction study is necessary.
It is important to treat carpal tunnel syndrome as early as possible since there are simple things you can do to make the problem go away while in the early stages. These simple actions include taking more frequent breaks to give your hands a rest, avoid activities that make symptoms worse, and apply a cold pack to reduce any swelling.
Other nonsurgical therapy options include wrist splinting and medications. Alternative options like yoga to help strengthen, stretch, and balance the body or hand therapy may reduce symptoms as well in some patients. Proper treatment typically relieves the tingling and numbness and restores hand and wrist function.
If pressure on the median nerve continues, it can lead to nerve damage and worsening symptoms. When symptoms are severe or don’t respond to treatments, surgery may be appropriate.
If you have concerns or think you may have carpal tunnel syndrome, request an appointment with one of our hand and wrist specialists: https://www.oaduluth.com/hand-and-wrist-specialists.php.
Understanding Arthritis
May 24, 2021
Not one single disease as commonly thought, “arthritis” is the informal way of referring to joint pain or a joint disease. With May being National Arthritis Awareness Month, we are taking this time to talk a little bit more about this very common, yet not very well understood diagnosis.
Common arthritis symptoms are joint pain and stiffness, redness, swelling, and decreased range of motion. Symptoms typically worsen with age and severe arthritis can make it difficult to do daily tasks, walk comfortably, and can result in chronic pain.
Types of Arthritis
The two most common types of arthritis are osteoarthritis and rheumatoid arthritis.
Osteoarthritis
Osteoarthritis, a degenerative arthritis and the most common type, is caused by wear and tear of your joints’ cartilage, the hard, slippery tissue that covers and protects the ends of bones where they form a joint.
Ideally, your cartilage cushions the ends of your bones and allows nearly frictionless joint motion. When damaged, you can experience bones grinding directly on another bone, causing pain and restricted movement. This damage can take place over many years or can be accelerated by a joint injury or infection.
The disorder commonly affects joints in the hands, knees, hips, and spine, however it can damage any joint in the body. Signs and symptoms of osteoarthritis include pain, stiffness, tenderness, swelling, a grating sensation, bone spurs, and loss of flexibility. Symptoms tend to develop slowly and worsen over time.
Rheumatoid Arthritis
Rheumatoid arthritis is a chronic inflammatory disorder where the immune system attacks the lining of the joint capsule, which is a tough membrane that encloses every part of the joint. The lining becomes inflamed and swollen. Over time, the disease can destroy cartilage and bone within the joint. The disorder can also affect other body systems including the skin, eyes, lungs, and blood vessels.
Signs and symptoms may include tender, warm, swollen, or stiff joints, and fatigue or fever and loss of appetite. Rheumatoid arthritis typically effects smaller joints first, and then spreads to larger joints throughout the body. These symptoms often vary in severity and may come and go.
Additional types of arthritis include infectious arthritis where a bacterium, virus, or fungus can enter the joint and cause inflammation, and metabolic arthritis where uric acid is formed as the body breaks down purines, a substance found in human cells.
Risk factors for arthritis include family history, age, gender, obesity, and previous joint injury.
Arthritis symptoms can be reduced through weight loss, exercise, heating pads or ice packs, and assistive devices. It is important to learn about the disease and treatment options if you believe you may have arthritis of any kind.
Diagnosis
It is important to talk with your doctor if you are experiencing joint pain. Before your appointment, start keeping notes of any signs and symptoms you are experiencing. During your appointment you will want to make sure to touch on when your symptoms started, which joints are painful, which activities make pain better or worse, and if you have any family history of joint pain.
In order to obtain a diagnosis, your doctor will check your joints for redness, warmth, and swelling. They may also suggest lab tests of body fluids in order to identify the type of arthritis you are living with. Your doctor may also request imaging, which can detect problems within your joint. Imaging tests could include x-rays, computerized tomography (CT scan), magnetic resonance imaging (MRI), or an ultrasound.
Treatments
Treatments can vary depending on the type of arthritis. Since damage to joints cannot be reversed, the goal of most treatments is to reduce and relieve symptoms, improve joint function, and increase the quality of life. No one option works best for every patient, so several different treatments or combination of treatments may be tested before the most successful is determined.
Examples of treatments are medications, physical therapy, and joint repair, replacement, or fusion surgery. You can learn more about total joint surgery services at Orthopaedic Associates at https://www.oaduluth.com/surgical.php.
If you are experiencing joint pain or arthritis symptoms, scheduling an appointment with one of our Board-certified surgeons could start you on the path to getting back to your normal lifestyle. Fill out a contact form today: https://www.oaduluth.com/contact.php.
Tips to Avoid Injury While Training for a Marathon
April 26, 2021
As the warm weather hits here in Duluth, runners throughout the area have one thing on their minds. The approaching Grandma’s Marathon. Whether competing against others or against yourself, the importance of safely training for race day is something everyone should be taking into consideration.
We talked to a few of our physical therapists about their training tips to avoid injury before and after running a marathon. Not making your way to the start line? Don’t worry. Following these tips can be beneficial for even casual runners.
Stretching
Our physical therapist team recommends dynamic stretching both before and after a run. These stretches are controlled movements that prepare and warm-up your body for performance. This helps with mobility, which is important for good running form. Static stretching, where you hold a single position for a period of time, can be beneficial after a run to increase flexibility and range of motion.
Strengthening exercises like core and hip movements can also be highly beneficial to complete after a run. Specific muscle strengthening is important in order to maintain good running form and to prevent injuries.
Different Types of Workouts while Training
Following a training program that incorporates a variety of intensities and distances is critical to improve cardiovascular fitness. Typically, a week should include at least one threshold workout, an intensity workout, and a long run at a lower heart rate.
Cross training and other endurance activities including biking, swimming, or skiing, between runs can help to prevent injuries.
While it is important to put in the miles while training for a marathon, strength training is also essential to avoid injury and improve performance. Plan to include core, hip, and single leg strengthening exercises, as well as working in different planes. For instance, use movements within the lateral and transverse planes instead of only the sagittal plane.
Doing bended and straight knee calf raises can also prevent calf strain, which effects almost every runner.
Universal Practices to Stay out of the PT’s Office
Most of the running injuries our therapists see are due to training error. Doing too much too soon can lead to injury, so progressions needs to be gradual. We recommend duration increases of 10% per week. Intensity can be safely increased at a rate of 3% per week.
When transitioning to different surfaces, for example from a treadmill to the road, it is important to keep your duration and intensity light for the first few runs since different muscles may be used depending on the terrain.
Make sure to keep hydration and fuel in mind. Eat about 40-60g of carbohydrates per hour during training and replenishing with at least 25g of protein and carbs after. Sleep can also be equally as important.
When to know you should see a Physical Therapist
If you feel any pain, monitor it over 24 hours. If the pain rates a 3 or 4 out of 10 during a run but goes back to a 0/10 within 24 hours, it is safe to continue running. If the pain gets worse during a run or over the next day, take a break from running for a few days. If the pain is from a tendon or muscle issue, try not to take more than a few days off. Otherwise you go into a pain – rest – weakness spiral. Tendons and muscles recover better with appropriate movement.
If you are having difficulty increasing weekly mileage due to pain, or symptoms persist after taking a few days off, then it is time to see a running specialist.
Good Tips for Marathon Day
Remember to be well hydrated and fueled by simple, easily digestible carbs before the race even starts (about 3 hours beforehand). Eat/refuel earlier in the marathon than you might think. If you allow yourself to go too far before consuming glucose, it may be difficult or impossible to catch back up to the fuel intake your body needs.
Also, remember to pace yourself! Don’t start out of the gate too fast or hard. Adrenaline will kick in when the race starts, but this jittery start will not be sustainable miles down the course.
Orthopaedic Associates Resources
Orthopaedic Associates of Duluth offers complete comprehensive running evaluations, which include a formal physical therapy evaluation and a running form assessment.
While training for any race - let alone a marathon - can be overwhelming, these tips should ease your mind and provide value to your running training program. Happy running!
Commonly Overlooked, SI Joint Dysfunction May Be the Cause of Your Back Pain
March 18, 2021
Are you experiencing pain, numbness, tingling, or weakness in your lower back, pelvis, or hips? Leg instability? Disturbed sleep or sitting patterns due to pain? Or pain going from sitting to standing, and have not been able to find a solution? Sacroiliac (SI) joint dysfunction is a commonly overlooked source of pain for many individuals.
What is Sacroiliac Joint Dysfunction?
The SI joint is located in the pelvis, linking the iliac bones (pelvis) to the sacrum (lowest part of the spine above the tailbone). The joint is an essential component for shock absorption to prevent impact forces from reaching your spine.
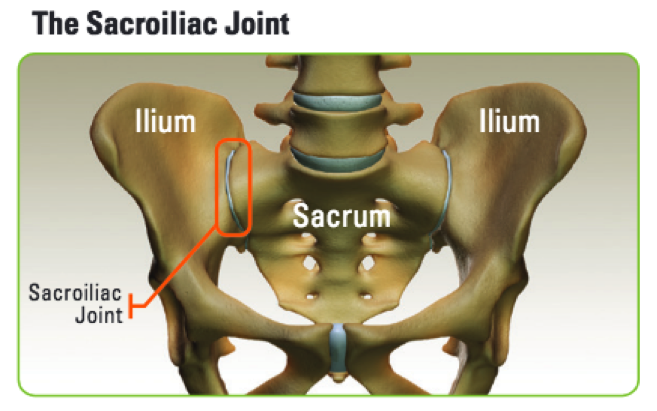
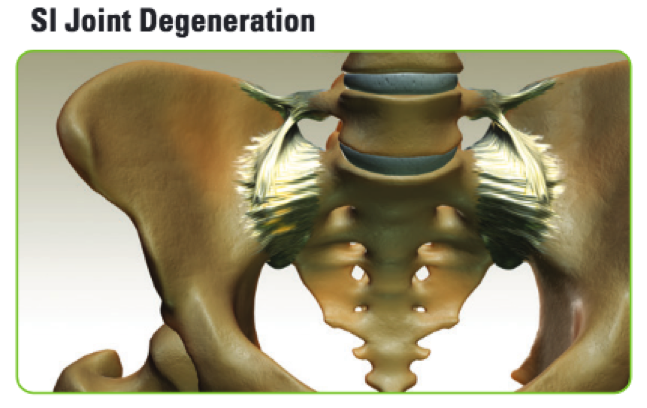
Like any joint in the body, the SI joint can be injured or become degenerative. SI joint dysfunction can cause back pain that may either be localized in your lower back or radiate all the way down through your buttocks and legs. This pain can range from mild to severe and often shows up while lifting, running, walking, or even sleeping on the involved side.
Clinical publications have identified the SI joint as a pain generator in 15-30% of chronic lower back pain patients. In addition, the SI joint is a pain generator in up to 43% of patients with continued or new onset lower back pain after a lumbar fusion.
There are several causes of SI joint dysfunction, so it can be difficult to pinpoint the primary issue. However, most common causes include injury due to an accident, triggering of pregnancy hormones, degenerative diseases such as osteoarthritis, and an inflammatory arthritis that primarily affects the spine called ankylosing spondylitis.
Making a Diagnosis
According to scientific data, it’s common for pain from the SI joint to feel like disc or lower back pain. For this reason, SI joint disorders should always be considered in lower back pain diagnosis.
A variety of tests performed during a physical examination may help reveal the SI joint as the cause of your symptoms. Sometimes, X-rays, CT-scan or MRI may also be helpful in the diagnosis of SI joint-related problems.
The most relied upon method to accurately determine whether the SI joint is the cause of lower back pain symptoms is to inject the SI joint with a local anesthetic. The injection will be delivered under either X-ray or CT guidance to verify accurate placement of the needle in the SI joint. If symptoms are decreased by at least 50%, it can be concluded that the SI joint is either the source of or a major contributor to the lower back pain.
Treatment
Once the SI joint is confirmed as the cause of symptoms, treatment can begin. Some patients respond to physical therapy, use of oral medications, or injection therapy. These treatments are often performed repetitively. If symptom improvement using these therapies only lasts temporarily, your surgeon may consider other options, including minimally invasive surgery.
If an SI joint fusion surgery is chosen as the next best course of action, Neurosurgeon Dr. Matthew T. Davies, MD is trained in the latest minimally invasive surgical technique, the iFuse Implant System from SI-Bone, Inc., which is proven to improve pain, patient function, and quality of life.
Join us on March 23 from 6-7 p.m. for a free patient educational webinar where Dr. Davies will discuss and review SI joint dysfunction. Click Here to Register

